Severe Melancholic Depression: Diagnose & Treatment Options

Melancholic depression is a severe subtype of major depressive disorder (MDD), often characterized by profound biological symptoms, significant functional impairment, and poor response to psychotherapy alone. Early recognition and appropriate treatment are essential to improve outcomes and reduce the risk of chronicity and suicidality.
🔍 Diagnosis: Recognizing Melancholia
According to DSM-5, melancholic features can be specified in MDD when one of the following is present:
- Loss of pleasure in all or almost all activities (anhedonia)
- Lack of reactivity to usually pleasurable stimuli
AND three or more of the following:
- Distinct quality of depressed mood (profound despondency or despair)
- Depression worse in the morning (diurnal variation)
- Early morning awakening (at least 2 hours before usual time)
- Marked psychomotor agitation or retardation
- Significant anorexia or weight loss
- Excessive or inappropriate guilt
💊 Treatment: Evidence-Based Strategies.
Let’s Begin by Answering this Question First

Time's up
Answer: Venlafaxine
1. Pharmacotherapy: Prioritize Antidepressants with Stronger Noradrenergic or Dopaminergic Activity
(a) SNRIs
- Example: Venlafaxine, Desvenlafaxine, Duloxetine
- May be more effective than SSRIs due to dual action.
(b) Bupropion
- Activating agent; consider if energy and motivation are significantly impaired.
(c) Tricyclic Antidepressants (TCAs)
- Example: Nortriptyline, Amitriptyline
- Often more effective than SSRIs in melancholic features but carry anticholinergic side effects.
(d) Avoid sole reliance on SSRIs
- SSRIs may be less effective in this population, particularly when marked anergia and psychomotor slowing are present.
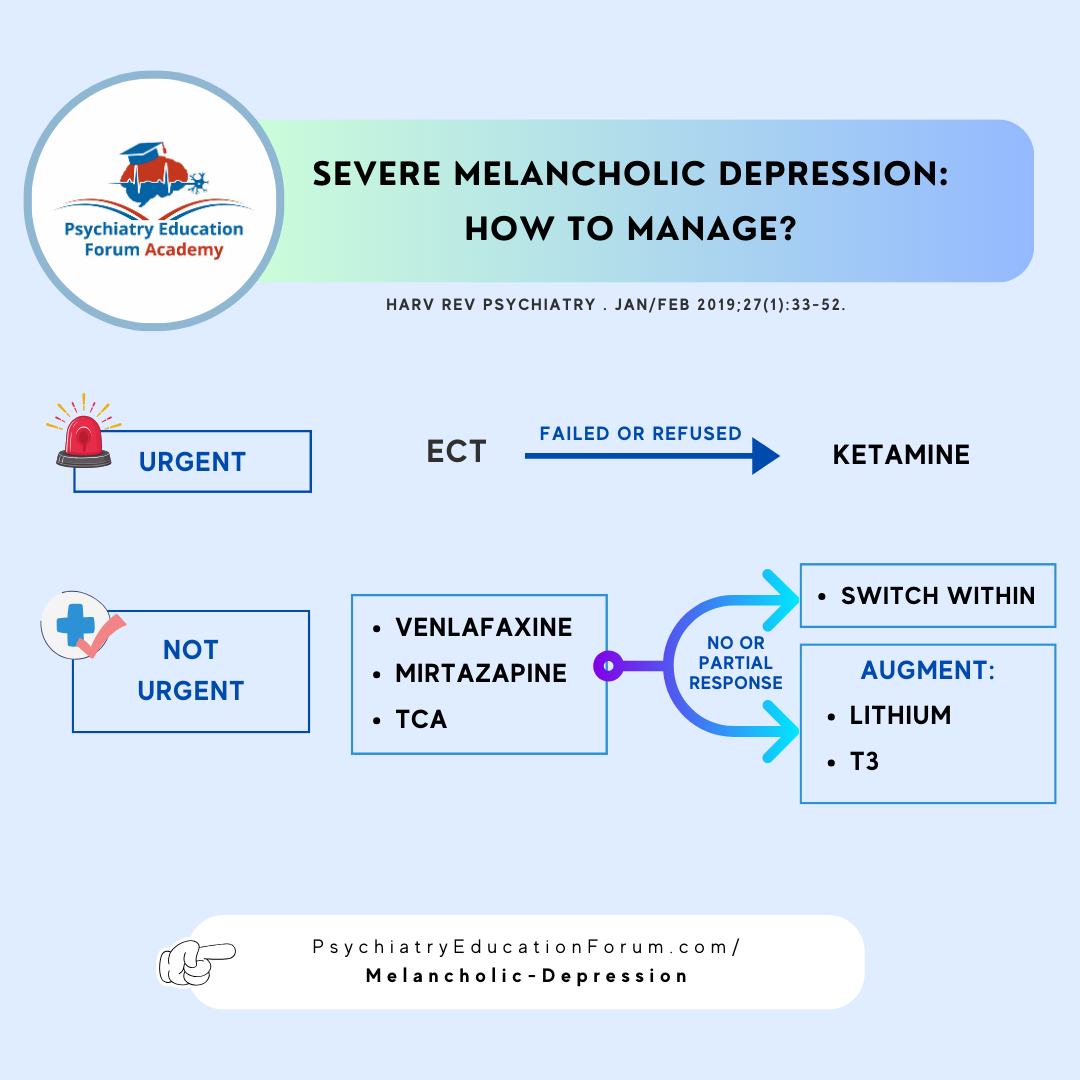
2. Electroconvulsive Therapy (ECT): Gold Standard for Severe or Treatment-Resistant Melancholia
High remission rates, particularly in:
- Psychotic depression
- Catatonia
- Severe suicidality
–> Should be considered early when rapid response is critical.
3. Augmentation Strategies
(a) Lithium augmentation
- can improve antidepressant response and reduce suicide risk.
(b) T3 (Triiodothyronine) augmentation
- Particularly helpful in patients with severe or treatment-resistant depression, including melancholic features.
- Mechanism: Enhances catecholaminergic transmission and may accelerate or potentiate antidepressant effects.
- Supported by studies (e.g., STAR*D trial) showing modest but clinically meaningful benefit, especially with tricyclics.
(c) Atypical Antipsychotics
- Useful for augmentation or when psychotic features are present
here is one slide from academy's lecture:
📌 Summary: Key Takeaways
Melancholic depression represents a biologically severe subtype of MDD that warrants aggressive treatment.
Pharmacological strategies should prioritize dual-acting antidepressants or TCAs over SSRIs.
ECT remains the most effective and underutilized treatment for severe or psychotic melancholic depression.
Early diagnosis, close monitoring, and multimodal treatment are essential for optimal outcomes.
FOR ACADEMY MEMBERS:
The Psychopharmacology Algorithm Project: An Update on Unipolar Nonpsychotic Depression.
This 45 minutes journal club video discussion will answer the following 11 clinically relevant questions:
- Which medications are first-line treatment options in the management of MDD [in outpatient setting]?
- What are the next step options after the first-line treatment fails (poor or no response): Augmentation options?
- What are the next step options after the first-line treatment fails (poor or no response): Switching options?
- Management options for Treatment-Resistant Depression without comorbidities.
- Management options for Treatment-Resistant Depression with and without Atypical Features.
- Management options for Treatment-Resistant Depression with Medical Comorbidities.
- Management options for Treatment-Resistant Depression with Chronic Pain.
- Management options for Treatment-Resistant Depression with OCD.
- Management options for Treatment-Resistant Depression with ADHD.
- Management options for Treatment-Resistant Depression with PTSD.
- How to manage Severe Melancholic Depression [in Inpatient Settings]?
We continue to review and summarize clinically relevant research to support your daily practice.
INTERESTED IN ACCESS TO THIS & OTHER CLINICALLY RELEVANT LECTURE SERIES?
JOIN ACADEMY MEMBERSHIP:
This is a closed membership for medical professionals only.
- 400+ Clinically Relevant Chapters: Each chapter within these sections is of direct clinical relevance for your daily practice. (Table of Content)
- Journal Club: we will post the most recently published psychiatry articles relevant to your daily clinical practice. (Read Content)
- Clinical Case Discussion: Dr. Singh (Psychiatry) and Dr. Kaur (Family Medicine) discuss clinical cases to integrate the clinical cases from Psychiatry and Medicine. (Read Content)
- Monthly Insights: Gain access to our monthly sessions featuring the latest on recent publications, new medication approvals, FDA updates, and more. (Monthly Insights)
- Discussion Forum & Community: Connect with other medical professionals and discuss your difficult-to-treat clinical cases. (Academy Network)
- Goal: is to have all important clinically relevant topics in one place for ease of access.
DISCOUNTS AVAILABLE FOR: Residents & Students ONLY.
Email us your student information (program information and way to confirm your student status) to: [email protected]
© 2026 All Rights Reserved.