ADHD Treatment During Pregnancy: What the Latest Evidence Means for Mothers and Clinicians
Want the latest research insights delivered straight to your inbox?
📊 Poll for Clinicians: We’d love to hear from you!
👉 Which ADHD medication do you most often use (or feel most comfortable prescribing) during pregnancy?
(a) 💊 Methylphenidate
(b) 💊 Amphetamines
(c) 💊 Atomoxetine
(d) ❌ Prefer not to prescribe during pregnancy
(Cast your vote in the comments section below!)
📌 Background
The use of ADHD medications during pregnancy is increasing worldwide. Concerns remain about their potential long-term effects on children, particularly the risk of neurodevelopmental disorders (NDDs) such as ADHD or autism spectrum disorder (ASD). While earlier studies suggested no significant risks, evidence has been limited and fragmented, especially for non-stimulants like atomoxetine.
🧪 Study Design
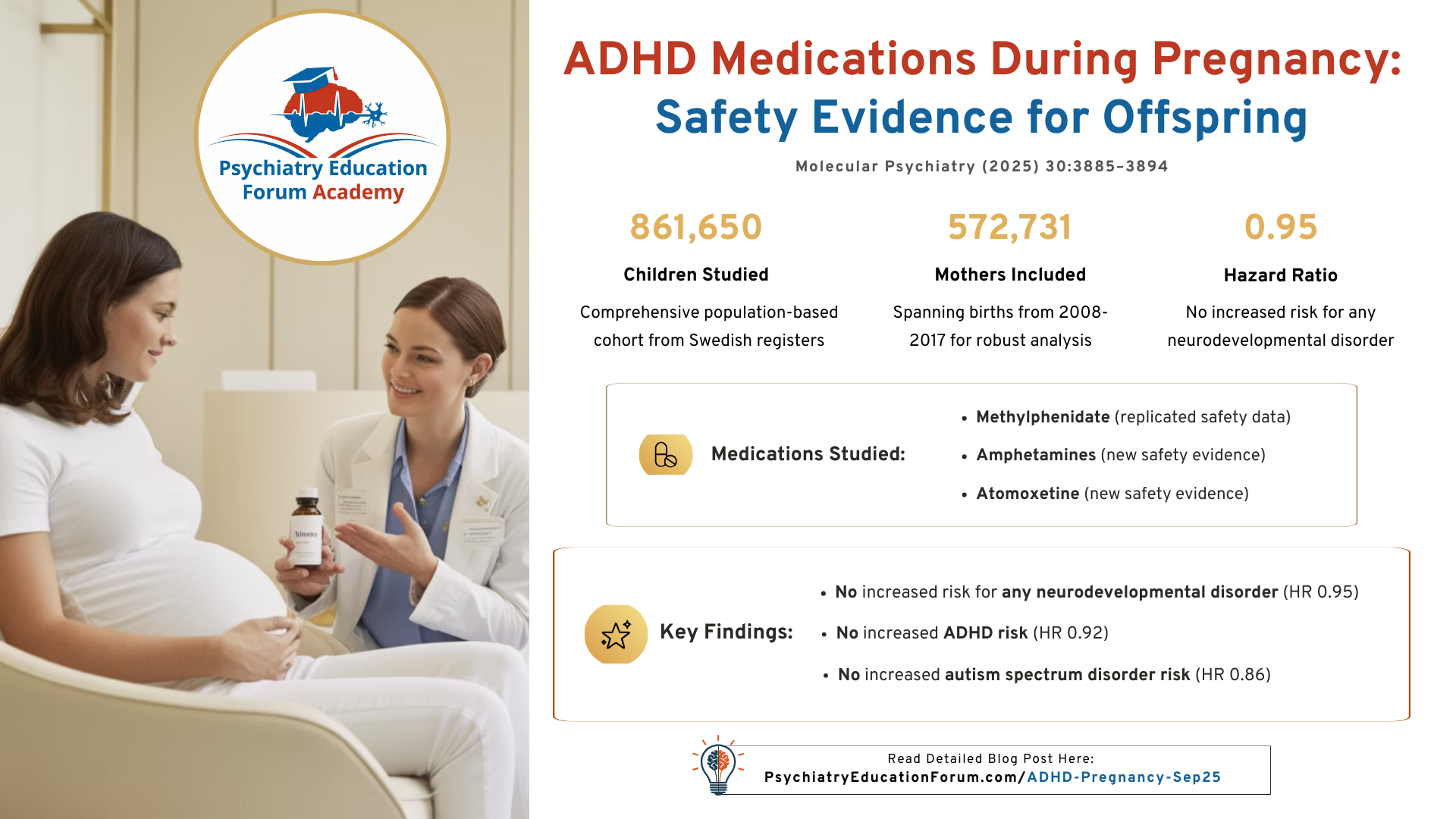
Population: 861,650 children born in Sweden (2008–2017)
Exposure groups:
Continued ADHD medication during pregnancy
Discontinued before pregnancy
Unexposed (no medication)
Medications studied: Methylphenidate, amphetamines (including lisdexamfetamine/dexamfetamine), and atomoxetine
Outcomes: Any NDD, ADHD, or ASD diagnosis in offspring (≥ age 3)
Analysis: Adjusted Cox regression, sibling comparison, and meta-analysis combining Swedish + Danish data
📊 Key Results
No increased risk of any NDD, ADHD, or ASD in exposed children compared to those whose mothers discontinued treatment:
Any NDD: HR 0.95 (95% CI 0.82–1.11)
ADHD: HR 0.92 (95% CI 0.78–1.08)
ASD: HR 0.86 (95% CI 0.63–1.18)
Consistent findings across:
Medication type (methylphenidate, amphetamines, atomoxetine)
Timing (1st, 2nd, 3rd trimester)
Duration of exposure
Meta-analysis (Sweden + Denmark): pooled HR for any NDD = 1.00 (95% CI 0.83–1.20)
🩺 Clinical Implications
Results provide reassurance that ADHD medications—including methylphenidate, amphetamines, and atomoxetine—do not increase long-term risk of NDDs in children.
Supports the view that women who require ADHD medication during pregnancy do not need to discontinue treatment solely out of concern for offspring neurodevelopmental outcomes.
Methylphenidate remains the best studied, but evidence for amphetamines and atomoxetine is now expanding.
Important for updating clinical guidelines and counseling expectant mothers with ADHD.
⚖️ Limitations
Possible residual confounding (e.g., maternal lifestyle, genetics).
Smaller sample sizes for amphetamines and atomoxetine.
Registry-based data may underestimate exposure if medication adherence was inconsistent.
✅ Clinical Takeaway
This large, robust population-based study confirms and extends prior findings:
- ADHD medication use during pregnancy does not increase the risk of long-term neurodevelopmental disorders in offspring.
- Clinicians can use this evidence to better guide discussions with patients balancing ADHD symptom management and pregnancy safety.
📚 References
- Madsen KB, Larsson H, Skoglund C, et al. In utero exposure to methylphenidate, amphetamines and atomoxetine and offspring neurodevelopmental disorders – a population-based cohort study and meta-analysis. Molecular Psychiatry. 2025;30:3885–3894 (article)
FOR ACADEMY MEMBERS:
WOMEN'S MENTAL HEALTH:
PREGNANCY, POST-PARTUM & PERI-MENOPAUSE
-
Antipsychotics
- Antipsychotics During Pregnancy & Postpartum
- Antipsychotics: Rates of Placental Passage
- Antipsychotics of Choice during Lactation
-
Antidepressants
- Zuranolone FDA Approved for Postpartum Depression
- Antidepressants During Pregnancy & Postpartum
- Antidepressants of Choice during Lactation
- RE104 for Postpartum Depression (2025 Data)
-
Mood Stabilizers
- Preconception Planning: Preparing for Pregnancy
- Continue or Discontinue Medication during Pregnancy & Postpartum?
- Lithium: During Pregnancy & Postpartum
- Lithium: use during Lactation
- Valproate: During Pregnancy & Postpartum
- Lamotrigine: During Pregnancy & Postpartum
- Other Mood Stabilizers: During Pregnancy & Postpartum
- Other Mood Stabilizers: use during Lactation
-
Benzodiazepines
- Benzodiazepines: During Pregnancy & Postpartum
-
ADHD Medication
- ADHD Medication & Brestfeeding
-
Postpartum Onset OCD
- Postpartum Onset OCD
-
Postpartum Psychosis
- Postpartum Psychosis: Evaluation & Management
-
Perimenopausal Depression
- Perimenopausal Depression
-
PMDD
- PMDD
Women’s Mental Health (Pregnancy, Post-partum & Peri-menopause)

Want the latest research insights delivered straight to your inbox?
We continue to review and summarize clinically relevant research to support your daily practice.
INTERESTED IN ACCESS TO THIS & OTHER CLINICALLY RELEVANT LECTURE SERIES?
JOIN ACADEMY MEMBERSHIP:
This is a closed membership for medical professionals only.
- 400+ Clinically Relevant Chapters: Each chapter within these sections is of direct clinical relevance for your daily practice. (Table of Content)
- Journal Club: we will post the most recently published psychiatry articles relevant to your daily clinical practice. (Read Content)
- Clinical Case Discussion: Dr. Singh (Psychiatry) and Dr. Kaur (Family Medicine) discuss clinical cases to integrate the clinical cases from Psychiatry and Medicine. (Read Content)
- Monthly Insights: Gain access to our monthly sessions featuring the latest on recent publications, new medication approvals, FDA updates, and more. (Monthly Insights)
- Discussion Forum & Community: Connect with other medical professionals and discuss your difficult-to-treat clinical cases. (Academy Network)
- Goal: is to have all important clinically relevant topics in one place for ease of access.
DISCOUNTS AVAILABLE FOR: Residents & Students ONLY.
Email us your student information (program information and way to confirm your student status) to: [email protected]
© 2026 All Rights Reserved.